Medical Tourism Blog
BPH (Benign Prostatic Hyperplasia) in Korea | Best Clinics, Costs, Procedure Types & More
Table of contents
- What Is BPH(Benign Prostatic Hyperplasia)?
- Best Clinics in Korea for Bphbenign Prostatic Hyperplasia
- Getting BPH(Benign Prostatic Hyperplasia) in Korea
- Cost of BPH (Benign Prostatic Hyperplasia) in Korea
- Alternatives to BPH(Benign Prostatic Hyperplasia)
- Conclusion
Considering treatment in Korea? Everything you need to know e.g. — how to avoid scams, visas, interpreters, recovery tips — in our Medical Tourism Master Guide. Plan with confidence in minutes, not weeks!
Benign prostatic hyperplasia (BPH) is a common, non-cancerous enlargement of the prostate that can affect urinary function as men age, and this article will help you understand it in the Korean context: we’ll start with what BPH is and how it’s identified, then walk you through getting evaluated and treated for BPH in Korea—covering care pathways, hospital options, and what to expect at appointments. We’ll clarify who typically needs assessment or treatment (and who may be suitable for watchful waiting), outline the expected costs of BPH care in Korea—from consultations and tests to medications and procedures—and explain how insurance factors in. Finally, we’ll explore alternatives for managing BPH, including lifestyle changes, medications, and minimally invasive options, to support informed decisions.
What Is BPH(Benign Prostatic Hyperplasia)?
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland that commonly affects men as they age. The prostate sits just below the bladder and surrounds the urethra like a doughnut. When it enlarges, it can compress the urethral channel and obstruct urine flow, leading to lower urinary tract symptoms (LUTS). Although BPH is not prostate cancer and does not transform into cancer, the two conditions can coexist and share overlapping symptoms, so proper evaluation is important.
Why the Prostate Enlarges
BPH reflects a gradual increase in both stromal (muscle and connective tissue) and epithelial (glandular) components, primarily within the transition zone of the prostate—the region that encircles the urethra. Key contributors include:
- Hormonal drivers: Dihydrotestosterone (DHT), converted from testosterone within the prostate, stimulates growth via androgen receptors. Shifts in the balance of androgens and estrogens with age may also promote hyperplasia.
- Growth factors and inflammation: Local signaling molecules and low-grade inflammation can accelerate cellular proliferation and tissue remodeling.
- Static vs dynamic components: “Static” obstruction arises from the bulk of enlarged tissue. “Dynamic” obstruction results from increased smooth muscle tone mediated by alpha-1 adrenergic receptors in the prostate and bladder neck.
How Common It Is
BPH is extremely common with advancing age. Many men develop microscopic (histologic) hyperplasia by their 50s, and the prevalence rises steadily thereafter. Lifestyle, metabolic health, and family history influence risk. While historically Asian men had smaller prostate volumes on average than Western populations, rapid demographic aging and lifestyle changes have made BPH and LUTS a frequent reason for urology visits in Korea.
Symptoms You Might Notice
BPH-related lower urinary tract symptoms are typically grouped as:
- Voiding (obstructive) symptoms: Hesitancy, weak or intermittent stream, straining, prolonged urination, and a sense of incomplete emptying.
- Storage (irritative) symptoms: Urgency, frequency, nocturia (waking at night to urinate), and urgency incontinence.
- Post-micturition symptoms: Dribbling after finishing and persistent feeling of residual urine.
Complications can include acute urinary retention (sudden inability to urinate), recurrent urinary tract infections, bladder stones, gross hematuria (visible blood in urine), bladder decompensation, and, in severe longstanding cases, hydronephrosis and kidney impairment.
Evaluation and Diagnosis
Assessment focuses on confirming BPH-related bladder outlet obstruction, gauging severity, ruling out other causes (e.g., infection, overactive bladder, urethral stricture, neurologic disease), and identifying risk of progression.
Common elements of evaluation:
- Symptom scoring: International Prostate Symptom Score (IPSS) with a quality-of-life question helps quantify severity and monitor response to therapy.
- History and physical exam: Includes a digital rectal exam (DRE) to estimate prostate size and check for nodules or asymmetry.
- Urinalysis ± culture: Screens for infection, blood, or other abnormalities.
- Prostate-specific antigen (PSA): Supports risk stratification and, with clinical judgment, helps decide if further evaluation for prostate cancer is needed. PSA also correlates with prostate volume; after 6+ months of a 5-alpha-reductase inhibitor, measured PSA is typically about half the true value.
- Uroflowmetry and post-void residual (PVR): Assess urinary flow rate and bladder emptying.
- Ultrasound: Transabdominal or transrectal imaging estimates prostate volume, detects bladder stones, and assesses kidneys if obstruction is suspected.
- Cystoscopy or urodynamics: Reserved for selected cases (e.g., hematuria, suspected strictures, prior pelvic surgery, mixed or unclear symptoms, planned intervention).
Risk factors for progression include large prostate volume (>30–40 mL), higher PSA (e.g., >1.5 ng/mL), older age, severe symptoms, and higher PVR.
Management Overview
Treatment is tailored to symptom severity, prostate size, risk of progression, and patient preferences—particularly regarding sexual function, medication tolerance, and willingness to undergo procedures.
- Watchful waiting and lifestyle
- Appropriate for mild symptoms or minimal bother.
- Behavioral strategies: Limit evening fluids, moderate caffeine and alcohol, time diuretics earlier in the day, double voiding, treat constipation, manage sleep apnea, maintain healthy weight, and exercise regularly.
- Regular follow-up: IPSS, PVR, and reassessment if symptoms worsen.
- Medications
- Alpha-1 blockers (e.g., tamsulosin, alfuzosin, silodosin, doxazosin, terazosin)
- Mechanism: Relax smooth muscle in the prostate and bladder neck to relieve dynamic obstruction.
- Onset: Days to 1–2 weeks; effective across prostate sizes.
- Side effects: Dizziness, orthostatic hypotension (less with uroselective agents), nasal congestion, ejaculatory dysfunction; rare intraoperative floppy iris syndrome during cataract surgery.
- 5-alpha-reductase inhibitors (5-ARIs) (finasteride, dutasteride)
- Mechanism: Block conversion of testosterone to DHT, shrinking the prostate ~20–25% over 6–12 months.
- Best for: Larger prostates (>30–40 mL) and men at higher risk of progression.
- Benefits: Reduce risk of urinary retention and need for surgery.
- Side effects: Decreased libido, erectile/ejaculatory dysfunction, gynecomastia; PSA drops ~50% after sustained use—clinicians adjust interpretation accordingly.
- Combination therapy (alpha-blocker + 5-ARI)
- Improves symptoms quickly and reduces long-term progression in men with larger glands and higher PSA.
- PDE5 inhibitors (tadalafil 5 mg daily)
- Improve LUTS and erectile dysfunction; avoid with nitrates and use caution with certain antihypertensives.
- Agents for storage-predominant symptoms
- Antimuscarinics (e.g., solifenacin) or beta-3 agonists (e.g., mirabegron) can be added to an alpha-blocker if PVR is reasonable; monitor for urinary retention.
- Desmopressin
- For nocturnal polyuria with bothersome nocturia; monitor sodium to avoid hyponatremia.
- Minimally invasive and surgical options Considered when medications fail, are not tolerated, or when complications occur (retention, recurrent infections, stones, bleeding, kidney impact).
- Office-based/minimally invasive procedures
- Prostatic urethral lift (UroLift): Implants retract lateral lobes to widen the urethra; rapid recovery; usually preserves ejaculation; ideal for prostates of moderate size without an obstructing median lobe.
- Water vapor thermal therapy (Rezūm): Steam ablates tissue over weeks; many retain ejaculation; transient irritative symptoms are common post-procedure.
- Temporary implantable nitinol device (iTind): Remodels the prostatic urethra over days; available in select centers.
- Prostatic artery embolization (PAE): Interventional radiology occludes prostatic arteries to shrink the gland; useful in large prostates or poor surgical candidates; variable availability and insurance coverage; outcomes depend on operator expertise.
- Legacy modalities (e.g., TUMT/TUNA) are less commonly used today.
- Transurethral surgery
- TURP (transurethral resection of the prostate): Long-standing standard; bipolar TURP reduces risk of TUR syndrome; effective for moderate-sized prostates.
- TUIP (transurethral incision of the prostate): For small prostates with high bladder neck; less bleeding and shorter time.
- Laser enucleation (e.g., HoLEP) and laser vaporization (e.g., GreenLight PVP): Effective across a wide size range; HoLEP is particularly well-suited for very large glands and is widely adopted in high-volume centers, including many hospitals in Korea.
- Open or robotic simple prostatectomy
- Reserved for very large prostates when endoscopic enucleation is not available or suitable.
Potential adverse effects of procedures include temporary urinary urgency/frequency, bleeding, infection, urethral stricture or bladder neck contracture, retrograde ejaculation (common after TURP and many surgeries), transient stress incontinence (especially after enucleation, usually improves), and, less commonly, erectile dysfunction.
When Urgent Care Is Needed
Acute urinary retention, high fever with urinary symptoms, visible blood with clots, severe flank pain, or signs of kidney dysfunction warrant urgent evaluation. In retention, bladder decompression with a catheter and an alpha-blocker are typical initial steps, followed by a trial without catheter and definitive management planning.
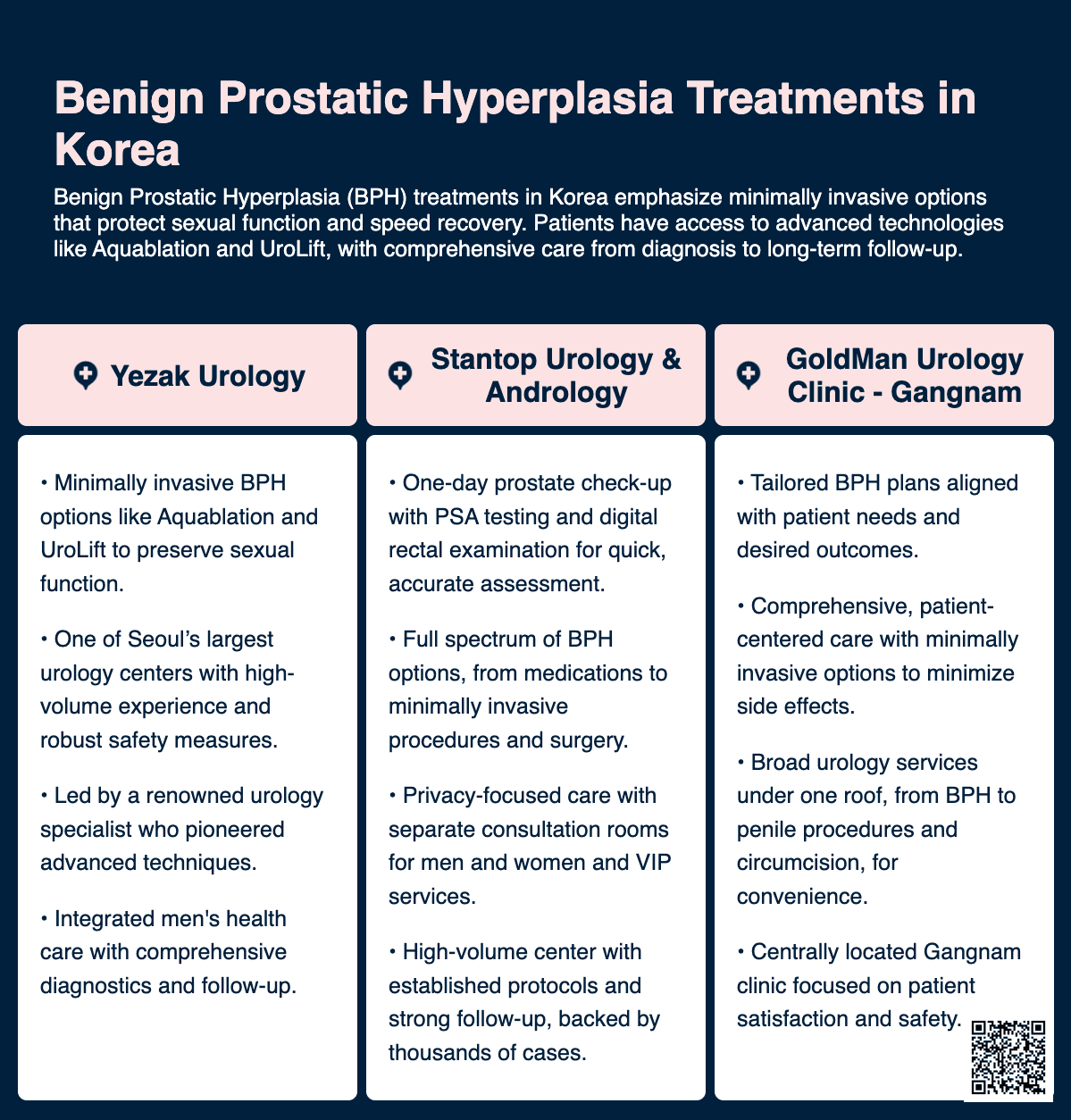
Best Clinics in Korea for Bphbenign Prostatic Hyperplasia
Listed below are the best clinics in Korea for bphbenign prostatic hyperplasia:
| Clinic Name | Key Features | Special Techniques |
|---|---|---|
| Stantop Urology & Andrology | - Specialized prostate care for BPH: Offers stepwise treatment options including medication, minimally invasive procedures, and surgery to relieve urinary symptoms caused by an enlarged prostate. - Rapid, thorough evaluation: Prostate One Day Check-Up enables fast, comprehensive assessment, including PSA testing and digital rectal examination. - Extensive experience you can trust: Built on more than 100,000 consultations and 40,000 surgeries performed, supporting consistent, expert decision-making for BPH management. - Recognized credibility: KBS-recognized clinic, reinforcing public trust and professional standing. - Privacy-first environment: Separate men’s and women’s consultation/treatment rooms help patients feel more comfortable discussing sensitive urologic symptoms. - Continuity of urologic care: Also diagnoses and treats related prostate conditions such as prostatitis, ensuring coordinated management when symptoms overlap. - VIP service option: Personalized care plans and dedicated facilities for patients seeking enhanced privacy, comfort, and tailored treatment pathways. | - Prostate One Day Check-Up - PSA testing - Digital rectal examination - BPH evaluation and treatment |
| GoldMan Urology Clinic - Gangnam | - GoldMan Urology Clinic – Gangnam clinic (Yangjae) provides patient-oriented urological care with an emphasis on advanced techniques designed to maximize postoperative satisfaction while minimizing complications and side effects. - Alongside procedures such as direct glans augmentation, artificial derma, autologous derma, silicone implants, and filler injections, the clinic also offers non-scalpel vasectomy and precise laser circumcision aimed at reducing bleeding and supporting faster recovery. - For men experiencing benign prostatic hyperplasia (BPH), GoldMan Urology Clinic offers tailored BPH treatment options based on individual patient needs, with the goal of achieving optimal outcomes. - The clinic’s broader focus on innovation, safety, and convenience supports comprehensive urologic care for patients seeking effective solutions in Gangnam. | - Direct glans augmentation - Artificial derma - Autologous derma - Silicone implants - Filler injections - Non-scalpel vasectomy - Precise laser circumcision - Tailored BPH treatment options |
| Proud Urology Clinic | - Proud Urology Clinic, established in 2016 in Korea, is a specialized men’s health center providing high-standard urologic care supported by JCI accreditation and professionally trained staff. - For men looking for reliable clinical guidance on common prostate health concerns such as benign prostatic hyperplasia (BPH), the clinic’s structured, patient-focused environment and emphasis on quality and safety can be an important starting point for evaluation and counseling. - The clinic offers a broad range of specialized services across men enhancement and reconstruction, including penis enlargement surgery, erectile dysfunction surgery (including penile implants), premature ejaculation treatment, vasectomy and vasectomy reversal, circumcision, penile curvature correction, vaseline removal, and scrotal reconstruction. - It also provides related men’s wellness services such as STD/STI testing and treatment and HPV vaccination, along with body-focused procedures like liposuction and male breast reduction, delivered by skilled professionals aiming to support patient confidence and well-being. | - Penis enlargement surgery - Erectile dysfunction surgery (including penile implants) - Premature ejaculation treatment - Vasectomy and vasectomy reversal - Circumcision - Penile curvature correction - Vaseline removal - Scrotal reconstruction - STD/STI testing and treatment - HPV vaccination - Liposuction - Male breast reduction |
Stantop Urology & Andrology
StanTop Urology & Andrology Clinic is a specialized urology and andrology medical institution focused on improving quality of life for patients in Korea and internationally through advanced, patient-centered care. With separate consultation and treatment rooms for men and women to maximize comfort and privacy, the clinic provides comprehensive prostate services—including BPH (benign prostatic hyperplasia) evaluation and treatment—supported by extensive clinical experience, KBS recognition, and a proven track record of over 100,000 patient consultations and 40,000 surgeries.
- Specialized prostate care for BPH: Offers stepwise treatment options including medication, minimally invasive procedures, and surgery to relieve urinary symptoms caused by an enlarged prostate.
- Rapid, thorough evaluation: Prostate One Day Check-Up enables fast, comprehensive assessment, including PSA testing and digital rectal examination.
- Extensive experience you can trust: Built on more than 100,000 consultations and 40,000 surgeries performed, supporting consistent, expert decision-making for BPH management.
- Recognized credibility: KBS-recognized clinic, reinforcing public trust and professional standing.
- Privacy-first environment: Separate men’s and women’s consultation/treatment rooms help patients feel more comfortable discussing sensitive urologic symptoms.
- Continuity of urologic care: Also diagnoses and treats related prostate conditions such as prostatitis, ensuring coordinated management when symptoms overlap.
- VIP service option: Personalized care plans and dedicated facilities for patients seeking enhanced privacy, comfort, and tailored treatment pathways.
You can check out their website here: Stantop Urology & Andrology Website
GoldMan Urology Clinic - Gangnam
GoldMan Urology Clinic – Gangnam clinic (Yangjae) provides patient-oriented urological care with an emphasis on advanced techniques designed to maximize postoperative satisfaction while minimizing complications and side effects. Alongside procedures such as direct glans augmentation, artificial derma, autologous derma, silicone implants, and filler injections, the clinic also offers non-scalpel vasectomy and precise laser circumcision aimed at reducing bleeding and supporting faster recovery.
For men experiencing benign prostatic hyperplasia (BPH), GoldMan Urology Clinic offers tailored BPH treatment options based on individual patient needs, with the goal of achieving optimal outcomes. The clinic’s broader focus on innovation, safety, and convenience supports comprehensive urologic care for patients seeking effective solutions in Gangnam.
Find more about this clinic here: GoldMan Urology Clinic - Gangnam Website
Proud Urology Clinic
Proud Urology Clinic, established in 2016 in Korea, is a specialized men’s health center providing high-standard urologic care supported by JCI accreditation and professionally trained staff. For men looking for reliable clinical guidance on common prostate health concerns such as benign prostatic hyperplasia (BPH), the clinic’s structured, patient-focused environment and emphasis on quality and safety can be an important starting point for evaluation and counseling.
The clinic offers a broad range of specialized services across men enhancement and reconstruction, including penis enlargement surgery, erectile dysfunction surgery (including penile implants), premature ejaculation treatment, vasectomy and vasectomy reversal, circumcision, penile curvature correction, vaseline removal, and scrotal reconstruction. It also provides related men’s wellness services such as STD/STI testing and treatment and HPV vaccination, along with body-focused procedures like liposuction and male breast reduction, delivered by skilled professionals aiming to support patient confidence and well-being.
Find more about this clinic here: Proud Urology Clinic Website
Special Considerations in Korea
- Care pathways: Many Korean urology clinics perform uroflowmetry and bladder scans at the first visit, enabling same-day assessment and treatment planning.
- Treatment availability: Alpha-blockers, 5-ARIs, combination therapy, and PDE5 inhibitors are widely prescribed. Laser enucleation (HoLEP) is commonly available at secondary and tertiary hospitals and is a popular choice for large prostates due to durable outcomes and shorter hospital stays.
- Insurance context: Under the National Health Insurance system, most standard evaluations and treatments for BPH (including TURP and HoLEP) are covered; coverage for newer minimally invasive therapies and PAE can vary by institution and indication.
- Cultural and lifestyle factors: High rates of late-night work and social dining can exacerbate nocturia and frequency. Attention to evening fluid/caffeine/alcohol intake and sleep hygiene often complements medical or procedural therapy.
Differentiating BPH from Other Conditions
- Prostate cancer: Typically asymptomatic early; may present with similar urinary symptoms later. PSA testing, DRE, and, when indicated, MRI/biopsy help differentiate.
- Prostatitis: Often includes pelvic/perineal pain and systemic symptoms; urinalysis/culture and examination guide diagnosis.
- Overactive bladder and neurogenic bladder: Predominantly storage symptoms, sometimes without obstruction; urodynamics may be needed.
- Urethral stricture: Weak stream and spraying; cystoscopy helps confirm.
Follow-Up
Ongoing monitoring aligns with the chosen therapy:
- Symptom tracking with IPSS and quality-of-life scores.
- PVR and uroflowmetry to assess objective response.
- PSA monitoring based on age, risk, and whether a 5-ARI is used.
- Post-procedural check-ins to manage transient symptoms and ensure proper recovery.
Understanding that BPH is a chronic, manageable condition helps set expectations. The choice among lifestyle measures, medications, minimally invasive procedures, and surgery is individualized, balancing symptom relief, durability, side effects, sexual function goals, and access to care.
Getting BPH(Benign Prostatic Hyperplasia) in Korea
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate that can obstruct urinary flow. Korea is a popular destination for BPH evaluation and treatment due to experienced urologists, high procedure volumes (especially for laser techniques), modern equipment, and efficient hospital pathways that accommodate both local and international patients.
Below is a detailed overview of how BPH is evaluated and treated in Korea, what to expect during the hospital journey, and practical considerations for those traveling for care.
Overview of the care pathway in Korea
- Access points: Patients typically enter via urology clinics within general or tertiary hospitals in major cities (e.g., Seoul, Busan, Daegu). Many centers have international patient offices and English-language support.
- Emphasis on minimally invasive surgery: Korean urologists widely perform endoscopic, laser-based procedures (especially HoLEP), with short hospital stays and rapid recovery.
- Efficient scheduling: After initial evaluation, procedures are often scheduled within days to a few weeks, depending on your health status and choice of hospital.
How BPH is diagnosed and staged in Korea
- History and symptom scoring: The International Prostate Symptom Score (IPSS) and quality-of-life questionnaires are standard.
- Physical exam: Digital rectal exam to assess size and consistency of the prostate.
- Laboratory tests: PSA (prostate-specific antigen) to screen for possible prostate cancer; urinalysis to check for infection or blood; kidney function.
- Uroflowmetry and post-void residual (PVR): Measures the strength of urine flow and how much urine remains in the bladder after voiding.
- Imaging: Transrectal or transperineal ultrasound for volume measurement; occasionally MRI if there are red flags for cancer or complex anatomy.
- Cystoscopy: Sometimes performed to assess urethra, bladder neck, and intravesical protrusion when planning surgery.
First-line (non-surgical) management commonly used in Korea
- Lifestyle: Fluid timing, reducing caffeine/alcohol, bladder training, managing constipation, review of medications that worsen symptoms.
- Medications:
- Alpha-1 blockers (e.g., tamsulosin, alfuzosin, silodosin) to relax prostate/bladder neck muscle and improve flow.
- 5-alpha-reductase inhibitors (finasteride or dutasteride) to shrink the prostate over months; useful for larger glands.
- Combination therapy for moderate to severe symptoms with enlarged prostates.
- Tadalafil (low dose) can improve lower urinary tract symptoms, particularly with erectile dysfunction.
- When to escalate: Recurrent urinary retention, recurrent UTIs, bladder stones, renal impairment, gross hematuria from BPH, severe or refractory symptoms, or patient preference.
Procedural options available in Korea Korean centers offer a broad spectrum of BPH procedures. Availability varies by institution; tertiary centers tend to offer the widest range. Your urologist will tailor the option to prostate size, anatomy, comorbidities, use of blood thinners, and your priorities (e.g., preserving ejaculation).
-
TURP (Transurethral Resection of the Prostate)
- What it is: Endoscopic shaving of obstructing prostate tissue via the urethra using monopolar or bipolar cautery.
- Anesthesia: Spinal or general.
- Hospital course: Typically 1–3 days; catheter for 1–3 days.
- Pros: Time-tested, broadly available, effective for moderate-size glands.
- Considerations: Bleeding risk, dilutional issues lower with bipolar systems; potential retrograde ejaculation; rare hyponatremia with older systems.
-
HoLEP (Holmium Laser Enucleation of the Prostate)
- What it is: Laser enucleation of the entire adenoma, with tissue morcellation in the bladder. Highly prevalent in Korea.
- Anesthesia: Spinal or general.
- Hospital course: Often 1 night; catheter typically removed within 24–48 hours.
- Pros: Works for any prostate size including very large glands; durable long-term outcomes with low retreatment rates; minimal bleeding.
- Considerations: Temporary urgency or stress incontinence in some patients during early recovery; retrograde ejaculation common.
-
Photoselective Vaporization of the Prostate (GreenLight laser)
- What it is: Laser vaporization of prostate tissue.
- Anesthesia: Spinal or general; sometimes short admissions or day surgery depending on hospital protocol.
- Pros: Less bleeding; useful for patients on certain anticoagulants (case-by-case).
- Considerations: Vaporization provides less tissue for pathology; may be less suitable for very large prostates.
-
Prostatic Urethral Lift (implant-based suspension)
- What it is: Implants retract prostatic lobes to open the urethra without cutting tissue.
- Anesthesia: Local, sedation, or light general; often outpatient.
- Pros: Fast recovery; minimal impact on sexual function and ejaculation for many patients.
- Considerations: Best for selected anatomies (e.g., minimal median lobe); symptom improvement may be more modest than tissue-removing procedures. Availability varies by center.
-
Water vapor thermal therapy (steam therapy)
- What it is: Radiofrequency-generated steam injections cause targeted tissue necrosis and shrinkage.
- Anesthesia: Typically office-based with local anesthesia and oral/IV sedation.
- Pros: Preserves sexual function in many; short procedure time.
- Considerations: Irritative symptoms for several weeks; gradual improvement over months. Availability can vary.
-
Prostate Artery Embolization (PAE)
- What it is: Interventional radiology procedure that reduces prostate blood flow, shrinking the gland.
- Anesthesia: Local with sedation.
- Pros: No urethral instrumentation; can suit patients unfit for anesthesia or with bleeding risks.
- Considerations: Symptom relief develops gradually; not ideal for all anatomies; retreatment rates can be higher than endoscopic surgery. Offered at select centers.
-
Simple Prostatectomy (open or robotic)
- What it is: Surgical removal of obstructing adenoma through an abdominal or robotic approach, typically reserved for very large prostates or when concurrent bladder surgery is needed.
- Anesthesia: General.
- Hospital course: Several days; longer catheterization than endoscopic options.
- Pros: Definitive for very large glands; allows simultaneous removal of bladder stones/diverticula.
- Considerations: Longer recovery; higher bleeding risk than endoscopic procedures.
-
Aquablation (waterjet ablation under robotic ultrasound guidance)
- What it is: Computer-guided high-velocity waterjet removes tissue while preserving surrounding structures.
- Anesthesia: General.
- Pros: Rapid resection; favorable sexual function profile in many.
- Considerations: Device availability varies by institution; requires specialized equipment and training.
How Korean teams choose a procedure
- Prostate size and anatomy: HoLEP or simple prostatectomy for very large glands; TURP/laser vaporization for small-to-moderate glands; implant/steam options for selected anatomies.
- Anticoagulation: Laser techniques and PAE may be considered for patients who cannot stop blood thinners; decisions individualized with cardiology/hematology input.
- Priority to preserve ejaculation: Implant-based and steam therapies can be considered when anatomy allows.
- Comorbidities and anesthesia risk: Office-based or IR options may be favored for higher-risk patients.
- Availability and surgeon expertise: Outcomes strongly correlate with surgeon and center experience; Korea has many high-volume HoLEP and TURP programs.
What to expect before the procedure
- Preoperative clearance: Blood tests, ECG, chest X-ray as needed, urine culture. Optimization of blood pressure, diabetes, and anticoagulation planning.
- Medication adjustments: Temporary pause or bridging of anticoagulants/antiplatelets is individualized. Alpha-blockers may continue; some centers start low-dose antibiotics based on urine culture.
- Informed consent: Discussion of benefits, alternatives, side effects (e.g., ejaculatory changes, temporary urgency, rare incontinence), and retreatment expectations.
- Logistics: Most hospitals provide a printed schedule; international offices assist with appointments, estimates, and interpreters.
Anesthesia and pain control
- Spinal anesthesia is common for endoscopic procedures; general anesthesia is also used based on patient preference, anatomy, and anesthesiologist recommendation.
- Postoperative pain is typically mild-to-moderate and managed with oral analgesics; bladder spasms can occur when a catheter is in place.
Hospital stay and recovery timeline (typical ranges)
- Length of stay: Same-day to 2 nights for endoscopic procedures; longer for open/robotic simple prostatectomy.
- Catheterization: 1–3 days for TURP/laser procedures; longer for simple prostatectomy; some minimally invasive options may be catheter-free or use short-term catheters.
- Early recovery (first 2–4 weeks): Expect frequency/urgency, mild burning, small clots, and activity limitations. Gradual improvement in stream and emptying.
- Return to activities: Light work in 1–2 weeks for endoscopic options; strenuous activity and heavy lifting typically avoided for 3–4 weeks (longer for open surgery).
- Sexual function: Retrograde ejaculation is common after tissue-removing procedures; erectile function is usually preserved but can be temporarily affected by discomfort or anxiety. Discuss priorities with your surgeon.
Risks and potential complications
- Common, usually temporary: Burning with urination, frequency/urgency, small clots, mild bleeding, bladder spasms.
- Procedure-related: Urinary tract infection, urinary retention, urethral stricture, bladder neck contracture, retrograde ejaculation; transient stress incontinence after enucleation procedures; rare persistent incontinence.
- Anesthesia-related: Nausea, headache (spinal), cardiopulmonary events in high-risk patients.
- Reintervention: Varies by technique and prostate size; enucleation and simple prostatectomy tend to have the lowest long-term retreatment rates.
Pathology and cancer considerations
- Tissue-removing procedures (TURP/HoLEP/simple prostatectomy) send chips/adenoma for pathology, which can occasionally detect incidental prostate cancer.
- Elevated PSA or suspicious imaging may prompt additional evaluation before BPH surgery.
Medications and supplies you may receive at discharge
- Short course of antibiotics if indicated by urine culture and hospital protocol.
- Pain control, bladder antispasmodics if needed.
- Alpha-blocker temporarily continued in some cases during early healing.
- Instructions for hydration, stool softeners, and activity.
Follow-up after you leave the hospital
- First check: Often 1–2 weeks for catheter status and symptom review (can be coordinated via telemedicine for international patients).
- Subsequent visits: 1–3 months with IPSS, uroflowmetry, and PVR. Additional visits as needed.
- When to call: Fever, inability to urinate, large clots, heavy bleeding, severe pain, or signs of infection.
Costs and coverage considerations
- Korean National Health Insurance (NHIS) covers eligible residents; international patients are typically self-pay.
- Charges depend on hospital type, length of stay, anesthesia, and device use. Bundled estimates are commonly provided through international offices.
- Ask for: Itemized quotation (surgeon, anesthesia, operating room, device fees, hospital stay), what happens if the length of stay changes, and fees for postoperative telehealth.
Tips for international patients
- Choosing a center: Look for high-volume urology departments with your preferred procedure and surgeon expertise. Many tertiary hospitals publish surgeon profiles and procedure counts.
- Documentation to bring: Symptom scores, medication list, prior imaging and lab results (PSA, uroflow, ultrasound/MRI), notes from your urologist, and any cardiac/anticoagulation guidance.
- Timing your trip: Plan to be in Korea a few days before surgery for work-up and 1–2 weeks after for early follow-up if possible. Some centers can compress this timeline.
- Language and support: Request an interpreter and a written care plan; most large hospitals can provide both.
- Travel after surgery: Avoid heavy lifting; ensure you have contact information for urgent issues and understand how to access care if you are flying soon after the procedure.
Questions to ask your Korean urologist
- Which BPH procedures do you offer and recommend for my prostate size and anatomy?
- What are the expected symptom improvements, side effects (especially ejaculation and continence), and retreatment rates for my case?
- How long will I need a catheter, how many nights in hospital, and when can I travel?
- What is the protocol for managing blood thinners?
- What will the total cost be, what is included, and how are complications billed?
- How will follow-up be handled once I return home?
Who is BPH(Benign Prostatic Hyperplasia) for?
- Men aged 40 and above—especially over 50—who notice lower urinary tract symptoms (weak stream, hesitancy, straining, dribbling, incomplete emptying, frequency, urgency, or waking at night to urinate)
- Men with a family history of prostate enlargement or urinary symptoms
- Men whose quality of life is affected by urinary issues, such as sleep disruption from nocturia, daytime frequency impacting work or travel, or anxiety about restroom access
- Men with health conditions linked to faster BPH progression, including metabolic syndrome, obesity, type 2 diabetes, hypertension, or dyslipidemia
- Men taking medications that can worsen urinary symptoms (e.g., decongestants with pseudoephedrine, certain antihistamines, tricyclic antidepressants)
- Men experiencing BPH-related complications such as recurrent urinary retention, repeated urinary tract infections, bladder stones, visible blood in urine, or kidney strain due to obstruction
- Men who have tried lifestyle changes or single medications without adequate relief and are considering combination therapy or procedural options
- Men who wish to preserve sexual or ejaculatory function and want treatments with lower sexual side-effect profiles
- Frail older adults or those with significant cardiovascular or anesthetic risks who may prefer minimally invasive or office-based procedures over major surgery
- Men found to have an enlarged prostate during a health check-up (via exam, ultrasound, or PSA testing) who also have urinary symptoms and need evaluation to distinguish BPH from other conditions
- Caregivers or partners seeking guidance to support someone dealing with nocturia, urgency, or incontinence related to BPH
- Men in Korea looking for care pathways that align with local practice, including IPSS symptom scoring, uroflowmetry, ultrasound-based prostate sizing, and access to insurance-covered medical and minimally invasive treatments
Cost of BPH (Benign Prostatic Hyperplasia) in Korea
Below is a practical overview of what patients can expect to spend for BPH evaluation and treatment in Korea and how that compares with other countries, including the United States. Figures vary by hospital tier, surgeon expertise, device use, and whether you are covered by Korea’s National Health Insurance (NHI) or paying as an international self-pay patient.
- Indicative high–low self-pay range in Korea: N/A–N/A
- Typical insured copay for Korean residents: lower than self-pay due to NHI benefits; international patients generally receive package/self-pay quotes.
- Key cost drivers in Korea:
- Treatment modality (medications vs office procedures such as UroLift/Rezūm vs surgical options such as TURP or HoLEP)
- Hospital tier (tertiary university hospitals and international clinics often price higher than community hospitals)
- Length of stay and anesthesia type
- Use of single-use devices and laser platforms (e.g., holmium laser)
- Pre-op imaging and lab bundles; post-op catheter care and follow-up
What you pay for in a typical BPH care pathway in Korea:
- Initial evaluation: urology consult, urinalysis, PSA, uroflowmetry, ultrasound ± MRI for select cases
- Medical therapy: alpha-blockers, 5-alpha-reductase inhibitors; monthly pharmacy costs vary by brand/generic
- Office-based procedures: minimally invasive therapies (e.g., Rezūm, UroLift) with device costs as major components
- Surgery: TURP, laser enucleation (e.g., HoLEP), with OR time, anesthesia, laser fiber, and hospitalization driving cost
- Aftercare: catheter supplies, follow-up visits, possible management of transient complications
How Korea compares with other countries (relative patterns)
- United States
- Self-pay prices for BPH procedures in the U.S. often exceed Korean self-pay by a substantial margin due to higher facility, anesthesia, and device fees.
- For common procedures (e.g., TURP, HoLEP, UroLift, Rezūm), U.S. cash prices are frequently higher than Korea’s by roughly 1.5× to 3× at major centers; prices can be even higher at brand-name hospitals in large metropolitan areas.
- Insurance in the U.S. can lower out-of-pocket costs, but deductibles and coinsurance may still exceed typical Korean self-pay quotes.
- Western Europe (e.g., Germany, UK, France)
- Public systems can keep out-of-pocket costs low for residents; private/self-pay prices at international hospitals often fall near or somewhat above Korean self-pay.
- Elective procedure wait times can be longer in public pathways; private fast-track options trend closer to or modestly above Korean quotes.
- Japan
- High-quality tertiary care with pricing that is generally comparable to or higher than Korean self-pay for international patients; residents benefit from national insurance.
- Advanced laser platforms are widely available; package quotes may trend slightly above similar Korean offerings.
- Singapore
- Private hospital pricing often exceeds Korean self-pay, especially for laser procedures and device-heavy minimally invasive options.
- Public sector pricing for residents is moderated by subsidies; international patient packages in private hospitals are commonly higher than Korean tertiary centers.
- Thailand
- International hospitals may offer package pricing that is similar to or lower than Korean community/secondary hospital pricing but often higher than Korea’s most cost-competitive centers.
- For complex laser procedures with very high-volume surgeons, Korea frequently remains price-competitive relative to top-tier international programs.
- India
- Self-pay packages for BPH surgery can be lower than in Korea, particularly at high-volume private centers.
- Device-heavy minimally invasive therapies may narrow the gap if imported disposables drive costs; surgeon and facility quality varies, with centers of excellence offering strong value.
Modality-specific cost expectations (relative, not absolute)
- Medications: lowest upfront cost; ongoing monthly expense
- Office procedures (UroLift, Rezūm): mid-range; driven by device cost; shorter recovery, often ambulatory
- TURP: mid-to-high; OR, anesthesia, 1–2 days hospital stay common
- HoLEP/laser enucleation: mid-to-high; laser disposables and OR time; often shorter catheterization and stay than TURP; outcomes depend on surgeon volume
- Additional items: imaging, labs, pathology, and management of comorbidities can add materially to the total
Practical tips for obtaining accurate Korean quotes
- Ask for itemized, all-in estimates: consults, pre-op testing, procedure, anesthesia, device/laser fees, hospital stay, medications, and follow-up.
- Clarify international patient pricing vs NHI-covered pricing; request self-pay packages tailored to your clinical plan (e.g., HoLEP vs TURP vs Rezūm/UroLift).
- Provide prostate size (via ultrasound/MRI), symptom severity, prior retention episodes, and current medications to help hospitals match you to the appropriate modality.
- Confirm expected length of stay and whether same-day discharge is feasible for your case.
- Check surgeon experience (e.g., annual HoLEP case volume) when comparing quotes at similar price points.
- Factor travel, lodging, and time off work into total cost of care when comparing Korea to other destinations.
Alternatives to BPH(Benign Prostatic Hyperplasia)
If you’re living in Korea and looking for options beyond long-term medication or conventional TURP (transurethral resection of the prostate), the following three approaches are commonly considered. The right choice depends on symptom severity, prostate size/shape, sexual function priorities, and access to experienced centers.
1) Watchful Waiting and Lifestyle Modification
Best for men with mild, tolerable lower urinary tract symptoms (LUTS) who want to avoid procedures or daily medications.
What it involves:
- Regular monitoring: symptom scoring (IPSS), urinalysis, PSA as indicated, and occasional uroflowmetry/post-void residual checks.
- Fluid timing: reduce evening fluids; avoid caffeine and alcohol that can worsen urgency and nocturia.
- Bladder strategies: double-voiding, timed voiding, and managing constipation to decrease straining.
- Medication review: avoid or adjust drugs that can worsen urinary retention (e.g., some decongestants, antihistamines).
- Comorbidity management: weight loss, diabetes control, treating sleep apnea can reduce nighttime urination.
- Pelvic floor and bladder training: can help urgency/frequency components.
Korean context:
- Most urology clinics and general hospitals in Korea offer structured monitoring with IPSS and uroflowmetry.
- This approach is low-cost, low-risk, and can be escalated to other options if symptoms progress.
Advantages:
- No procedure, no anesthesia, minimal risk.
- Suitable for patients prioritizing safety and simplicity.
Considerations:
- Does not reduce prostate size; symptoms may gradually worsen over time.
- Requires adherence to behavioral measures and follow-up.
2) Minimally Invasive Office-Based Therapies (UroLift/Rezūm)
For men with moderate symptoms who want more relief than lifestyle measures provide but prefer to avoid conventional surgery.
Two common options:
-
Prostatic Urethral Lift (UroLift, 유로리프트): tiny implants retract enlarged prostate tissue away from the urethra without cutting or heating.
- Ideal candidates: prostates roughly 30–80 mL, no obstructive median lobe.
- Benefits: quick recovery, usually preserves ejaculation, often done under local anesthesia.
- Considerations: not suited for very large glands; some patients need retreatment over time.
-
Water Vapor Thermal Therapy (Rezūm, 레쥼): controlled steam injections shrink obstructive prostate tissue.
- Ideal candidates: prostates about 30–80 mL; can treat some median lobes.
- Benefits: durable symptom relief for many, low impact on sexual function, outpatient procedure.
- Considerations: transient urinary urgency/burning is common; short-term catheter use is typical; possible retreatment.
Korean context:
- Availability is expanding at tertiary centers in Seoul and major cities; uptake varies by hospital.
- Pre-procedure evaluation typically includes IPSS, ultrasound for prostate size, uroflowmetry, and PSA as indicated.
- Insurance coverage and out-of-pocket costs differ; confirm details with your hospital.
Advantages:
- Faster recovery and fewer sexual side effects than many surgical options.
- Can reduce or eliminate the need for daily medications.
Considerations:
- Not ideal for very large prostates or complex anatomy (varies by method).
- A minority will require additional treatment within several years.
3) Holmium Laser Enucleation of the Prostate (HoLEP, 홀렙)
A definitive surgical alternative to TURP and open/simple prostatectomy, especially effective for larger prostates.
What it is:
- A laser “enucleates” the obstructing adenoma from the prostate capsule through the urethra, then the tissue is removed and sent for pathology.
- Effective across a wide range of sizes, including very large glands (>80–100 mL).
Who it suits:
- Men with moderate-to-severe symptoms, urinary retention, recurrent infections from obstruction, bladder stones, or failure of medication/minimally invasive therapies.
- Patients who want long-lasting relief with low retreatment rates.
Advantages:
- Strong, durable symptom improvement; low risk of bleeding compared to TURP.
- Short catheterization time and hospital stay in most cases.
- Suitable for anticoagulated patients in many centers, with appropriate planning.
Considerations:
- Requires anesthesia; temporary urinary urgency, burning, or stress incontinence can occur during recovery.
- Retrograde ejaculation is common; discuss sexual function priorities beforehand.
- Outcomes depend on surgeon experience.
Korean context:
- Widely available in Korea at both tertiary and community hospitals; many centers have high-volume HoLEP experience.
- Standard preoperative workup includes prostate sizing (ultrasound/MRI as needed), uroflowmetry, and PSA evaluation.
Conclusion
In summary, BPH is a common, non-cancerous enlargement of the prostate that can significantly affect quality of life, and Korea offers a strong mix of advanced diagnostics, experienced urologists, and streamlined care pathways for those seeking evaluation and treatment. Men with bothersome lower urinary tract symptoms—especially over age 50 or those not responding to lifestyle measures or medication—are typical candidates, though the best approach depends on symptom severity, prostate size, and health status. In Korea, treatment options range from watchful waiting and medications to minimally invasive therapies (such as Rezum or UroLift) and definitive surgeries (including TURP or HoLEP), with costs varying by hospital, technology, and insurance or international patient packages. If you are considering care in Korea, compare centers’ expertise and outcomes, confirm transparent pricing and support services, and discuss alternatives—like continuing medical therapy or less invasive procedures—with a urologist so you can match effectiveness, recovery time, and budget to your goals.










