Medical Tourism Blog
Genital Pain from Tucking MTF? Penile Inversion Vaginoplasty Solutions in Korea

Table of contents
- Understanding Genital Pain and Discomfort from Tucking (MTF)
- What is Tucking and its Significance?
- Common Causes and Symptoms of Tucking-Related Pain and Irritation
- Potential Health Risks and Side Effects Associated with Prolonged Tucking
- Common Pseudonyms and Community Terminology for Genitalia and Tucking
- Practical Tips for Safer Tucking Practices and When to Consult a Healthcare Provider
- Penile Inversion Vaginoplasty: A Detailed Medical Overview
- The Patient Journey: Getting Penile Inversion Vaginoplasty in South Korea
- Costs and Financial Planning for Medical Tourists
- Average Costs of Penile Inversion Vaginoplasty in South Korea
- Detailed Breakdown of What is Typically Included in the Surgical Package
- Comparative Analysis of PIV Costs: South Korea vs. Other Popular Medical Tourism Destinations
- Additional Expenses to Consider (Beyond the Surgical Package)
- Considerations for Insurance Coverage and Financing
- Patient Experiences and Outcomes: Relief from Tucking Pain
- How PIV Directly Addresses and Resolves Chronic Genital Pain and Discomfort Caused by Tucking
- Patient-Reported Satisfaction with Aesthetic, Functional, and Psychosocial Outcomes
- Expected Recovery Timeline: Managing Discomfort, Swelling, and Mobility
- Discussion of Potential Post-operative Complications and How They are Managed
- Impact on Quality of Life, Self-Esteem, and Resolution of Gender Dysphoria
- Conclusion: Making an Informed Decision for Your Well-being
Considering treatment in Korea? Everything you need to know e.g. — how to avoid scams, visas, interpreters, recovery tips — in our Medical Tourism Master Guide. Plan with confidence in minutes, not weeks!
This guide is crafted for transfeminine individuals dealing with chronic genital pain or discomfort from tucking and considering Penile Inversion Vaginoplasty (PIV) as a long-term solution. Our goal is to offer clear, reliable, and compassionate information to help you make informed decisions about this significant medical procedure.
Tucking is a common practice among transfeminine people—including trans women, transfemme, and non-binary individuals—where the penis and testicles are positioned to create a flatter, smoother appearance in the crotch area. Many tuck to ease gender dysphoria, feel more comfortable in clothing, and boost self-confidence. The need for gender affirmation and social safety often outweighs immediate physical comfort, creating a tough balance between psychological and physical well-being. In this context, surgical options like PIV can offer a permanent solution to both physical discomfort and underlying dysphoria.
Understanding Genital Pain and Discomfort from Tucking (MTF)
What is Tucking and its Significance?
Tucking involves moving the penis and testicles to achieve a smoother genital appearance. Typically, the testicles are gently pushed into the inguinal canals, and the penis is pulled back between the legs, secured with tight underwear, gaffs, or medical-grade tape. For many, tucking is more than a cosmetic choice—it’s a vital part of gender affirmation, helping reduce body dysphoria, increase comfort and confidence, and lessen anxiety about being “read” in public.
Common Causes and Symptoms of Tucking-Related Pain and Irritation
While tucking can be affirming, it may also cause pain and irritation. Common causes include skin chafing from friction or tight garments, warm and moist environments that promote bacterial or fungal growth, poor hygiene, improper taping (especially with non-medical tape), and excessive tightness or prolonged tucking that restricts blood flow.
Symptoms can range from mild discomfort to more serious issues. Reported side effects include itching (28%), rash (21%), testicular pain (17%), penile pain (14%), skin infections, and urinary tract infections (UTIs). Other signs include soreness, tightness, urinary pain, and overheating. If you experience pain, numbness, or skin discoloration, it’s important to untuck immediately to prevent complications.
Potential Health Risks and Side Effects Associated with Prolonged Tucking
Prolonged tucking can lead to several health risks. Increased testicular temperature may cause heat stress and impact fertility; in some cases, stopping tucking has led to the return of sperm production. Other risks include restricted blood flow, numbness, and nerve damage. About 65% of those who tuck report at least one side effect, with gonad pain being the most common (32%). The risk increases with longer daily tucking durations.
Despite the prevalence of side effects, only 10% seek medical care, even though 70% feel comfortable discussing tucking with their provider. This gap suggests barriers in healthcare access or proactive inquiry. Some may fear judgment, leading to silent suffering. Healthcare providers need to create affirming, non-judgmental spaces and proactively discuss tucking to catch issues early and prevent chronic problems.
Common Pseudonyms and Community Terminology for Genitalia and Tucking
While medical professionals use terms like “penis,” “scrotum,” and “testicles,” community language often includes “girldick,” “clit,” “ladybits,” or “shenis” for the penis, and “the testes*” for testicles. This guide respects the diverse terminology individuals use for their bodies.
Practical Tips for Safer Tucking Practices and When to Consult a Healthcare Provider
To reduce discomfort and health risks, take regular breaks from tucking—ideally every 4-8 or 8-12 hours—and never sleep while tucked. Maintain good hygiene, use only medical-grade tape, tuck gently, and avoid overly tight garments.
See a healthcare provider if symptoms persist or worsen, especially if you notice signs of infection or ongoing pain. If you have fertility concerns, discuss them with your doctor. While self-care can help, persistent irritation may require medical intervention. For many, tucking is a temporary or long-term coping strategy, but chronic pain may prompt consideration of permanent surgical solutions like vaginoplasty. Chronic tucking pain can be a direct medical reason for surgery, alongside gender affirmation.
Table 1: Common Side Effects and Symptoms of Tucking
| Symptom/Side Effect | Reported Prevalence | Description/Impact |
|---|---|---|
| Itching | 28% | Skin irritation from friction or moisture |
| Rash | 21% | Skin inflammation from chafing or infection |
| Testicular Pain | 17% (32% overall) | Discomfort, possible heat stress or restricted blood flow |
| Penile Pain | 14% | Discomfort in the penis |
| Skin Infections | Increased risk | Bacterial/fungal growth in warm, moist environment |
| Urinary Tract Infections (UTIs) | Increased risk | May result from altered anatomy or hygiene issues |
| Discomfort/Soreness | Common | General unease or tenderness |
| Tightness | Common | Constriction from garments or tape |
| Urinary Pain | Common | Discomfort during urination, often linked to UTIs or irritation |
| Overheating | Common | Increased genital temperature, may impact fertility |
| Numbness | With excessive tightness | Loss of sensation from restricted blood flow or nerve compression |
| Skin Discoloration | With restricted blood flow | Changes in skin color, may indicate circulation issues |
Penile Inversion Vaginoplasty: A Detailed Medical Overview
What is Penile Inversion Vaginoplasty (PIV) and its Primary Objectives?
Penile Inversion Vaginoplasty (PIV) is the most widely used and accepted surgical technique for creating a neovagina in transfeminine individuals. The main goals are to construct an anatomical, aesthetically pleasing, and functional vagina and vulva—enabling normal urination, preserving sexual sensation, and allowing for receptive sexual intercourse, all while minimizing scarring. The ideal neovagina is secretory, flexible, hairless, and pink, with a typical depth of 4-7 inches (6-10 cm) and a diameter of 1-1.5 inches. PIV is a major reconstructive surgery, not a minor cosmetic procedure, and understanding its complexity helps set realistic expectations.
Expected Aesthetic and Functional Outcomes, Including Sexual Sensation
After PIV, patients can expect a functional vagina that looks similar to a natal vagina, with adequate depth and width. Sexual sensation is preserved by creating a small, sensate clitoris from part of the glans penis, keeping its nerve and blood supply intact for erogenous sensation and orgasm. Normal urination while sitting is achieved by shortening and repositioning the urethra. The prostate is usually left in place and can contribute to sexual sensation.
Key Stages of the Surgical Procedure
PIV is a complex surgery, usually performed by a plastic surgeon and a urologist.
- Pre-operative Preparation: Permanent hair removal is recommended for the neovaginal lining area, or hair follicles are cauterized during surgery. Estrogen therapy may be paused about a month before surgery to reduce the risk of deep vein thrombosis.
- Patient Positioning: The patient is placed in the lithotomy position.
- Incision and Dissection: An incision is made in the perineal area to create a tunnel for the new vaginal canal. A penoscrotal flap and butterfly incision are used to harvest scrotal skin.
- Scrotal Skin Graft Preparation: The harvested skin is prepared, fat removed, and hair follicles cauterized. The skin is then tubularized over a vaginal dilator. If there’s not enough skin, grafts from other areas or a tunica vaginalis mucosal graft may be used.
- Orchiectomy: Both testicles are removed, allowing for reduced testosterone blockers after surgery.
- Penectomy and Penile Inversion: The penis is degloved, and the skin is inverted to line the new vaginal cavity. Erectile tissue is removed.
- Creation of the Neovaginal Space: A space is dissected between the rectum, prostate, and bladder, sometimes using robotic assistance and peritoneal flaps for added depth and lubrication.
- Clitoris Reconstruction (Clitoroplasty): A sensate clitoris is created from the glans penis, preserving nerves and blood supply.
- Urethral Repositioning (Urethroplasty): The urethra is shortened and moved to the female anatomical position.
- Labiaplasty: The labia minora and majora are constructed from available skin.
- Closure and Post-operative Devices: The vaginal walls are sutured, drains placed, and gauze packing with antibiotics is inserted. A urinary catheter is kept for several days, and a vaginal dilator or mould is used to maintain depth. Lifelong dilation is essential for success.
Variations in Technique
While PIV is the most common, there are single-stage and two-stage procedures. Robotic-assisted peritoneal flap vaginoplasty is a newer option for deeper canals and possible lubrication. For those with insufficient skin or anatomical considerations, intestinal-based techniques may be used, though these have their own risks. Patients should understand both the transformative benefits and the realistic risks of complications.
Table 2: Key Surgical Steps of Penile Inversion Vaginoplasty
| Phase | Specific Action/Procedure | Purpose/Detail |
|---|---|---|
| Pre-operative | Hair Removal | Prevent hair growth in neovagina |
| Hormone Therapy Suspension | Reduce DVT risk | |
| Surgical Steps | Patient Positioning | Lithotomy position for access |
| Incision & Dissection | Create tunnel for neovagina | |
| Scrotal Skin Graft Prep | Prepare skin for neovaginal lining | |
| Orchiectomy | Remove testicles to stop testosterone | |
| Penectomy & Inversion | Invert penile skin to line vagina | |
| Neovaginal Space Creation | Dissect space for vaginal canal | |
| Clitoris Reconstruction | Create sensate clitoris | |
| Urethral Repositioning | Move urethra to female position | |
| Labiaplasty | Construct labia from available skin | |
| Post-operative Devices | Closure & Drains | Suture tissues, place drains |
| Vaginal Packing | Maintain shape and healing | |
| Urinary Catheter | Assist urination during healing | |
| Vaginal Dilator/Mould | Maintain neovagina depth |
The Patient Journey: Getting Penile Inversion Vaginoplasty in South Korea
Best Clinics in Korea for Genital Pain From Tucking Mtf
Listed below are the best clinics in Korea for genital pain from tucking mtf:
| Clinic Name | Key Features | Special Techniques |
|---|---|---|
| Kangdong Sacred Heart Hospital LGBTQ Plus Center | Inclusive, patient-centered care for LGBTQ+ community; Comprehensive medical procedures and therapies; Emphasis on respect and diversity; Specialized mental health counseling; Hormone therapy management (including fertility preservation); Plastic and reconstructive surgeries (top surgery, breast augmentation, facial feminization); Care addressing genital pain from tucking (MTF) | Gender-affirming treatments; Voice training; STI prevention and treatment; Specialized mental health counseling for LGBTQ+; Multidisciplinary care (psychiatry, surgery, otolaryngology, infectious diseases) |
| Kangdong Sacred Heart Hospital | Comprehensive specialized procedures; Highly qualified multidisciplinary team; State-of-the-art facility; Innovation in patient-centered care; Inclusive, privacy-conscious environment for transgender patients; Commitment to education and individualized care plans; Reputation for excellence in surgery and pain management | Advanced diagnostic tools for genital pain assessment; Minimally invasive and non-surgical options; Integrated pain management; Expertise in transgender care (urology, reconstructive surgery, mental health); Multidisciplinary, supportive approach |
Kangdong Sacred Heart Hospital LGBTQ Plus Center
Kangdong Sacred Heart Hospital LGBTQ Plus Center in Cheonho is a leading healthcare provider specializing in inclusive, patient-centered care for the LGBTQ+ community in Korea. The center offers a comprehensive range of medical procedures and therapies, with a strong emphasis on respect and diversity to foster a healthier society. Among its services are specialized mental health counseling tailored for LGBTQ+ individuals, hormone therapy management including fertility preservation, as well as plastic and reconstructive surgeries such as top surgery, breast augmentation, and facial feminization.
The clinic is also equipped to address issues such as genital pain from tucking for transfeminine individuals (MTF), recognizing the unique healthcare challenges faced by this community. With skilled professionals in psychiatry, surgery, otolaryngology, and infectious diseases, the Center provides a safe and understanding environment where patients can discuss their needs openly—from gender-affirming treatments and voice training to STI prevention and treatment. The Kangdong Sacred Heart Hospital LGBTQ Plus Center stands out as a vital resource for comprehensive and compassionate care for those navigating gender affirmation and associated health concerns.
Find more about this clinic here: Kangdong Sacred Heart Hospital LGBTQ Plus Center Website
Kangdong Sacred Heart Hospital
Kangdong Sacred Heart Hospital, located in Cheonho, is a leading medical institution renowned for its comprehensive range of specialized procedures delivered by highly qualified professionals in a state-of-the-art facility. The hospital embraces innovation and patient-centered care, ensuring the highest standards in both general and highly specialized medical services. Patients benefit from the expertise of a multidisciplinary team, access to advanced technology, and a supportive environment focused on comfort and recovery.
Why Kangdong Sacred Heart Hospital is the Best Choice for Genital Pain From Tucking Mtf:
- Highly qualified physicians experienced in both urology and the care of transgender individuals
- Advanced diagnostic tools for accurate assessment of genital pain and related complications
- Comprehensive, multidisciplinary support including pain management, mental health, and reconstructive expertise
- Privacy-conscious and inclusive environment sensitive to the unique needs of transgender patients
- Access to the latest minimally invasive and non-surgical treatment options
- Strong commitment to patient education, empowerment, and individualized care plans
- Reputation for innovation and excellence in surgery, pain management, and overall patient experience
With its integrated approach and the support of expert clinicians from multiple specialties, Kangdong Sacred Heart Hospital stands out as a top destination in Korea for those seeking safe, compassionate, and effective care for genital pain related to tucking in Mtf individuals.
Find more about this clinic here: Kangdong Sacred Heart Hospital Website
Why South Korea is a Popular Destination for Gender-Affirming Surgery
South Korea is a top choice for gender-affirming surgeries thanks to advanced techniques, skilled surgeons, modern facilities, and competitive pricing. Many clinics offer comprehensive packages—including accommodation, transportation, and pre- and post-op care—making the process smoother for international patients. Specialized LGBTQ+ centers and multidisciplinary teams provide holistic support, making South Korea’s medical tourism ecosystem especially attractive.
Step-by-Step Guide for International Patients
The typical journey for international patients seeking Penile Inversion Vaginoplasty in South Korea includes:
- Initial Consultations and Evaluations: Consultations with mental health professionals, endocrinologists, and surgeons. Patients must meet eligibility criteria, often following WPATH guidelines, including documented gender dysphoria, informed consent, age of majority, and usually at least 12 months of hormone therapy. Psychological evaluations and health screenings (blood tests, ECG, X-rays, MRI, bone density) are standard.
- Booking and Deposit: Once approved, patients book their surgery date, usually with a 10% deposit.
- Travel and Accommodation: Patients arrange visas, flights, and accommodation, often with clinic assistance. A stay of several weeks is typical to cover pre-op, surgery, and initial recovery. Accommodation costs range from $50 to $150 per night.
- Hospital Stay and Immediate Post-op Care: Surgery is performed under general or regional anesthesia. Patients stay in the hospital for 5-7 nights for monitoring and pain management, with a urinary catheter in place for up to 10 days.
- Follow-up and Long-term Recovery: Follow-up appointments monitor healing. Patients receive instructions on hygiene, activity restrictions, and vaginal dilation (initially 4 times a day, then less frequent for life). Full recovery takes weeks to months, with sexual activity restricted for 4-6 weeks or longer.
Overview of Reputable Clinics and Hospitals in South Korea Offering PIV
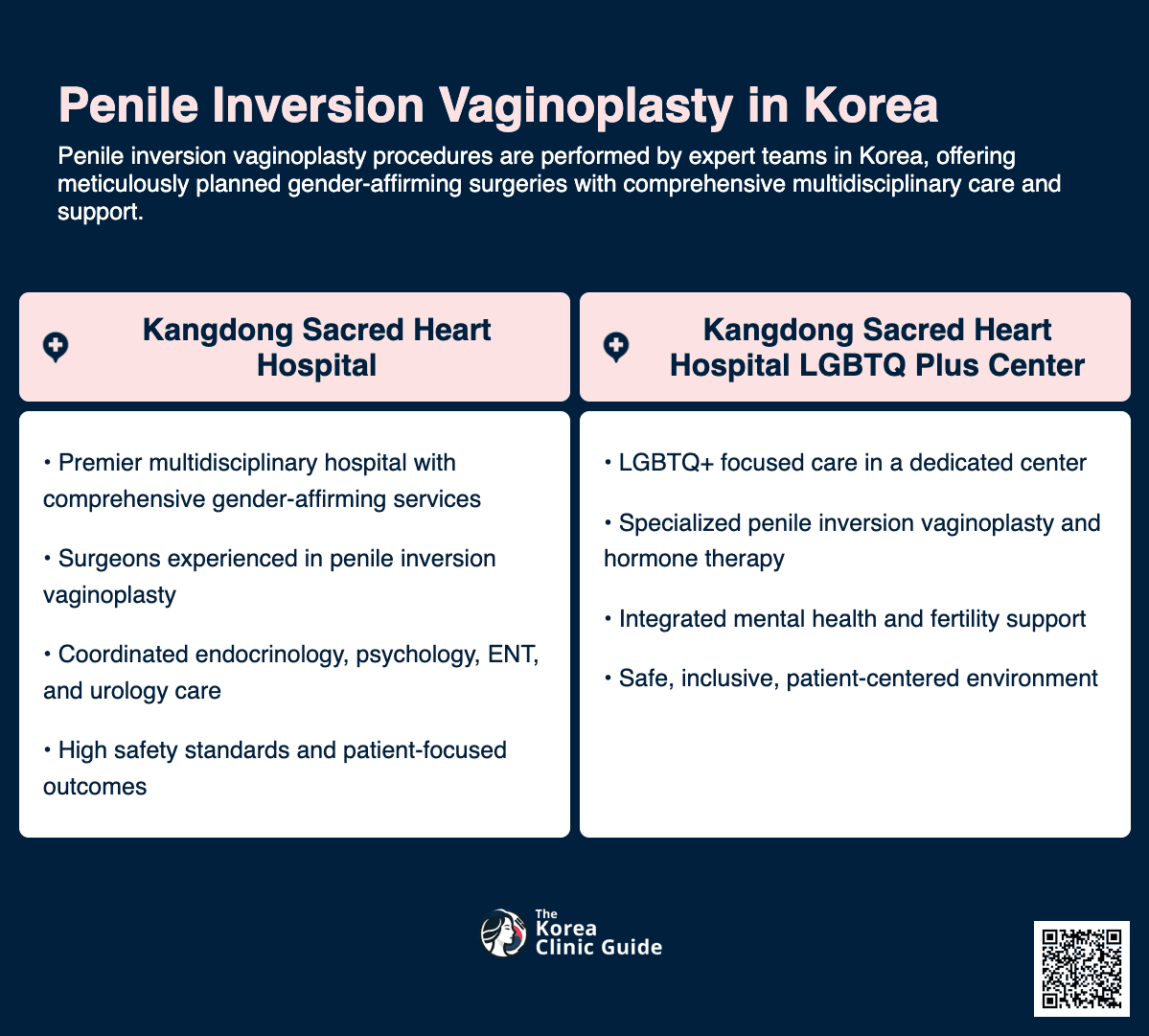
- Kangdong Sacred Heart Hospital (LGBTQ+ Center): Known for advanced care and expertise in gender-affirming surgeries, with a multidisciplinary LGBTQ+ center offering mental health, hormone therapy, and surgical services.
- PS Beauty Clinic: Offers a wide range of cosmetic and gender-affirming procedures, using advanced technology and a personalized approach.
Table 3: Patient Journey for Penile Inversion Vaginoplasty in South Korea (for International Patients)
| Phase | Key Steps/Actions | Estimated Duration/Timing | Important Considerations |
|---|---|---|---|
| Pre-operative Evaluation | Consultations (Mental Health, Endo, Surgical Team) | Weeks to months | WPATH guidelines, hormone therapy duration |
| Health Screenings | Before travel or upon arrival | Assess health and readiness | |
| Surgical Procedure | Booking & Deposit | Upon approval | 10% deposit to secure date |
| Travel Logistics | Weeks to months before | Plan for several weeks’ stay | |
| Surgery | 6-10 hours | Specialized surgeons | |
| Immediate Post-op Care | Hospital Stay | 5-7 nights | Pain management, bed rest, catheter |
| Initial Follow-ups | 1-2 weeks post-op | Monitor healing | |
| Long-term Recovery | Dilation Training & Practice | Begins before discharge, lifelong | Maintain depth (e.g., 4x/day initially) |
| Continued Follow-ups | As advised | Monitor outcomes, address complications | |
| Full Recovery & Activity | 6 weeks to months | Gradual return to work, exercise, sex |
Costs and Financial Planning for Medical Tourists
Average Costs of Penile Inversion Vaginoplasty in South Korea
Penile Inversion Vaginoplasty in South Korea typically costs $8,500 to $17,000 USD. Other sources cite ranges from $5,000 to $15,800 USD. For overall MTF surgery (including other procedures), costs are usually $10,000 to $20,000 USD.
Detailed Breakdown of What is Typically Included in the Surgical Package
Most Korean clinics offer comprehensive packages for medical tourists, often including:
- Hospital stays
- Follow-up appointments
- Pre-operative assessments (psychological, counseling, medical tests)
- Consultation fees
- Post-surgery dressing and wound care supplies
A 10% deposit is usually required to secure the surgery date.
Comparative Analysis of PIV Costs: South Korea vs. Other Popular Medical Tourism Destinations
- United States: Vaginoplasty costs $8,000–$20,000; overall MTF surgery $15,000–$50,000 or more.
- United Kingdom: MTF surgery $12,000–$25,000; high standards but possible long wait times.
- Thailand: Vaginoplasty $12,000–$14,500; overall GRS $8,000–$25,000; lower prices but variable expertise and aftercare.
- Mexico: Sex reassignment surgery ~$8,500; MTF SRS $5,000–$10,000.
- Germany: MTF surgery $10,000–$20,000; high-quality care.
- India: Gender Confirmation Surgery $8,000–$12,000; affordable.
- Singapore: $50,000–$60,000; significantly higher costs.
South Korea offers a balance between cost and quality, with integrated care and robust aftercare, making it a “sweet spot” for many patients.
Additional Expenses to Consider (Beyond the Surgical Package)
- Flights: $700–$1,500 round-trip to Seoul.
- Accommodation: $50–$150 per night for several weeks.
- Additional Tests: Blood tests, ECG, X-rays ($700–$1,000); MRI ($900–$1,200); Bone Density ($750–$1,000).
- Hormone Therapy: $300–$600 if not covered by insurance.
- Personal Expenses: Daily living, transportation, and unforeseen costs.
These extra costs can add thousands to your total budget, so careful planning is essential.
Considerations for Insurance Coverage and Financing
Insurance coverage for vaginoplasty varies by country and policy. Check with your provider about coverage for medically necessary procedures. Some clinics or third-party lenders may offer financing. While lower prices may be tempting, consider the reputation of the clinic and surgeon, the quality of care, and aftercare support. The cheapest option isn’t always the best value for such a life-changing procedure.
Table 4: Penile Inversion Vaginoplasty Cost Comparison by Country (USD)
| Country | Estimated Cost Range (USD) | Key Inclusions/Exclusions | Noteworthy Considerations |
|---|---|---|---|
| South Korea | $8,500–$17,000 (PIV); $10,000–$20,000 (overall MTF) | Often includes hospital stay, follow-ups, pre-op assessments | Cost-effective, high-quality, WPATH standards |
| United States | $8,000–$20,000 (Vaginoplasty); $15,000–$50,000 (overall MTF) | Varies by provider | Higher costs |
| United Kingdom | $12,000–$25,000 (overall MTF) | High standards | Possible long wait times |
| Thailand | $12,000–$14,500 (Vaginoplasty); $5,000–$15,000 (overall MTF) | Excludes flights/accommodation | Competitive pricing, variable expertise |
| Mexico | ~$8,500 (SRS); $5,000–$10,000 (MTF SRS) | Affordable | |
| Germany | $10,000–$20,000 (overall MTF) | Comprehensive care | High-quality, experienced surgeons |
| India | $8,000–$12,000 (GCS) | Affordable | |
| Singapore | $50,000–$60,000 (GRS) | Significantly higher costs |
Patient Experiences and Outcomes: Relief from Tucking Pain
How PIV Directly Addresses and Resolves Chronic Genital Pain and Discomfort Caused by Tucking
Penile Inversion Vaginoplasty offers a permanent solution for chronic scrotal skin irritation and genital pain from tucking by removing the source of irritation. Post-surgery pain is usually well-controlled with medication and subsides within days to a couple of weeks, marking a significant improvement in quality of life.
Patient-Reported Satisfaction with Aesthetic, Functional, and Psychosocial Outcomes
Studies show high satisfaction rates after PIV. One study found 94% of patients “felt positively about their genitals” and would “do this operation again,” with overall satisfaction averaging 91%.
- Aesthetic Outcomes: High satisfaction with neovagina depth, width, and appearance.
- Functional Outcomes: High satisfaction with urination, continence, sexual intercourse, and clitoral sensitivity.
- Psychosocial Outcomes: 71% report resolution of gender dysphoria, with many feeling more comfortable, confident, and satisfied with their sexual and social lives. Relief from chronic tucking pain greatly enhances quality of life.
Expected Recovery Timeline: Managing Discomfort, Swelling, and Mobility
- Hospital Stay: 5–7 days, starting with bed rest and then gradual movement.
- Immediate Post-op (1–2 weeks): Swelling, soreness, and bruising are common but improve within one to two weeks. Pain is managed with medication.
- Return to Activities (2–6 weeks): Most return to work in 1–2 weeks; light exercise resumes in 2–4 weeks. Sexual activity is restricted for 4–6 weeks or longer.
- Full Recovery: Usually within six weeks if post-op care is followed.
- Aiding Recovery: Ice packs reduce swelling, loose clothing prevents irritation, and sanitary pads (not tampons) should be used until fully healed.
While the main goal is relief from chronic pain, recovery involves temporary discomfort. Pre-op counseling should cover pain management and the possibility of prolonged pain.
Discussion of Potential Post-operative Complications and How They are Managed
PIV carries a moderate risk of minor complications; about half of patients experience at least one.
- Common Complications:
- Granulation tissue (26%)
- Intravaginal scarring (20%)
- Prolonged pain (20%)
- Stenosis/strictures (11%)
- Tissue necrosis (4%)
- Fistula (1%)
- Temporary altered sensation
Most minor complications are managed with local care. Persistent or severe issues require surgical follow-up. Regret rates are very low (~2%), highlighting the profound benefits of gender affirmation and pain relief.
Impact on Quality of Life, Self-Esteem, and Resolution of Gender Dysphoria
Most patients report improved quality of life and self-esteem after PIV. Aligning physical appearance with gender identity is deeply affirming, reducing distress from dysphoria and chronic pain. This surgery is not just a physical treatment but a crucial step in holistic gender affirmation.
Table 5: Patient-Reported Outcomes and Satisfaction with Penile Inversion Vaginoplasty
| Outcome Category | Specific Outcome | Satisfaction Level | Common Complications & Frequencies |
|---|---|---|---|
| Aesthetics | Vagina Depth | 4.7/5 (72.2% Very Satisfied) | Granulation Tissue (26%) |
| Vagina Width | 4.7/5 (72.2% Very Satisfied) | Intravaginal Scarring (20%) | |
| Genitalia Appearance | 4.5/5 (61.1% Very Satisfied) | Prolonged Pain (20%) | |
| Labia Majora/Minora Appearance | 4.4/5 (55.6% Very Satisfied) | Stenosis/Strictures (11%) | |
| Clitoris Appearance | 4.6/5 (72.2% Very Satisfied) | Tissue Necrosis (4%) | |
| Functional | Urination | 4.2/5 (44.4% Very Satisfied) | Fistula (1%) |
| Urinary Stream Direction | 4.1/5 (55.6% Very Satisfied) | Temporary/Rarely Permanent Sensation Changes | |
| Urinary Stream Force | 4.9/5 (88.9% Very Satisfied) | ||
| Urinary Continence | 4.4/5 (61.1% Very Satisfied) | ||
| Defecation | 4.8/5 (83.3% Very Satisfied) | ||
| Bowel Continence | 5/5 (100% Very Satisfied) | ||
| Sexual Intercourse | 4.3/5 (38.9% Very Satisfied) | ||
| Orgasms | 4.2/5 (72.2% Very Satisfied) | ||
| Clitoris Sensitivity | 4.8/5 (88.9% Very Satisfied) | ||
| Psychosocial | Satisfaction with Self | 4.8/5 (88.9% Very Satisfied) | |
| Satisfaction with Others | 4.3/5 (61.1% Very Satisfied) | ||
| Satisfaction with Sexual Life | 4.5/5 (38.9% Very Satisfied) | ||
| Resolution of Gender Dysphoria | 71% reported resolution | ||
| Global | Overall Process Satisfaction | 4.8/5 (77.7% Very Satisfied) | Moderate risk of minor complications |
| Satisfaction with Surgery Choice | 4.9/5 (94.4% Very Satisfied) | Low regret rates (~2%) |
Conclusion: Making an Informed Decision for Your Well-being
Penile Inversion Vaginoplasty is a highly effective, transformative option for transfeminine individuals experiencing chronic pain from tucking, offering both physical relief and profound gender affirmation. While the procedure requires thorough preparation, understanding of the surgical process, and a lifelong commitment to dilation, most patients report significant improvements in quality of life and self-esteem. South Korea stands out as a destination for high-quality, integrated care at competitive prices, but careful planning for all associated costs is essential. Ultimately, the decision to pursue PIV should be made with trusted healthcare professionals, considering all medical, financial, and personal factors.
References
1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40









